Prohibition of Discrimination in Health Care
Employer Action Items
Employer plan sponsors should monitor all legal developments in consultation with benefits counsel and work closely with their benefits advisors in complying with their Section 1557 obligations. The latest updates can be found on the Department of Health and Human Services’ (HHS) Office of Civil Rights’ (OCR) Section 1557 webpage. Employers should understand the types of discrimination prohibited by Section 1557 and should familiarize themselves with the steps employees follow to file a complaint under Section 1557 guidelines. In particular, employers should:
- Speak with insurers and third-party administrators to understand whether, and to what extent, the coverage provided is offered in compliance with the non-discrimination requirements, as detailed in the 2024 HHS rulemaking. In doing so, it should be kept in mind whether the plan is fully insured or self-insured as well as whether the plan itself receives federal financial assistance.
- Confirm that, absent a religious freedom and conscious exemption, the plan does not enforce a blanket restriction or any types of nominal restrictions prohibiting plan-level coverage of healthcare benefits related to the treatment of gender dysphoria, particularly respecting surgical interventions arising in the context of affirmation of gender identity.
- Considering gender dysphoria is a mental health disorder as set out in a manual published by the American Psychiatric Association, understand, and consider the impacts associated with the Mental Health Parity & Addiction Equity Act (MHPAEA) as related to any quantitative and/or nonquantitative treatment limitations imposed upon benefits and services related to the treatment of gender dysphoria.
- Understand the Section 1557 complaint process, including submission, evaluation, retaliation, and disposition.
- Step 1. Employee files a complaint with OCR if the employee believes they have been subjected to discrimination based on race, color, national origin, sex, age, gender identity or disability in a covered health program or activity (for more information related to the filing and/or enforcement of submitted complaints, please see here: here).
- Step 2. OCR will promptly inform the employee if they have the jurisdiction to investigate the claim.
- Step 3. If OCR is not the proper entity due to jurisdiction, OCR may provide other federal agencies with jurisdiction and OCR will forward the complaint to the proper agency.
- Step 4. If OCR is the proper enforcing entity, OCR will vet the complaint with a specific intake process and provide an initial evaluation of the complaint.
- Step 5: Upon reply from the Complainant (the employee) and the Respondent (the employer), if probable cause exists respecting a violation of Section 1557, OCR will fully investigate the Complainant’s allegations.
- Step 6: Upon performance of its investigation, OCR will prepare an enforcement report detailing its determination as to the complaint, along with an assessment of resulting damages and/or civil monetary penalties to the Respondent (appeal rights are also detailed as a matter of due process).
Please note that Section 1557 also prohibits any form of retaliation related to the filing of any discrimination complaint. When investigating a complaint, OCR informs all recipients as to the prohibition against retaliation. In addition, during the complaint process, OCR will seek the complainant’s consent to reveal their identity or identifying information, if necessary, to investigate the complaint. Consent is voluntary, and it is not always needed to investigate a complaint. Failure to provide consent, however, may make it difficult to investigate some aspects of the complaint.
Overview
Section 1557 of the Affordable Care Act (ACA) prohibits discrimination based on race, color, national origin, sex, age or disability in certain health programs and activities. Section 1557 has been in effect since its enactment in 2010, with the OCR enforcing the provision. The tenets of Section 1557 generally apply to any health program or activity that receives federal financial assistance. On April 26, 2024, HHS issued a final rule under 1557, which is scheduled to be published on May 6, 2024, and will take effect 60 days later. The effective dates may vary for certain provisions of the rule (please see the chart in #4 of these FAQs).
Prior rules and guidance that the OCR published to implement Section 1557 have been the subject of numerous lawsuits, dating back to when initial regulations were issued in 2016. The litigation has primarily focused on:
- Which health programs and activities are subject to Section 1557’s nondiscrimination requirements; and
- Whether sex discrimination includes discrimination based on gender identity, sexual orientation, and termination of pregnancy.
Under final regulations from 2020, gender identity and pregnancy termination were not included in the definition of sex discrimination, and the scope of Section 1557 was narrower than the 2016 regulations (namely, health insurance issuers were not generally included).
Prior rules and guidance published since 2016 by the OCR became the subject of several lawsuits in multiple jurisdictions. For example, the 4th Circuit Court of Appeals (governing the federal districts located in Maryland, North Carolina, South Carolina, Virginia, and Virginia) recently published a decision holding that state health insurance plans must provide coverage for gender-affirming care, including surgical interventions. Litigation from other state and federal jurisdictions has primarily focused on:
- Which health programs and what activities are subject to Section 1557’s nondiscrimination requirements; and,
- Specifically, what types of discrimination are prohibited by Section 1557, and under what specific circumstances, including:
- Healthcare benefits and services primarily related to the treatment of gender dysphoria or affirmation of an individual’s selected gender identity;
- Healthcare benefits and services primarily related to the termination of a pregnancy; and
- Regulatory requirements related to employer mandates to address identification and workplace treatment of persons with disabilities (e.g., evaluation of ameliorate aids, appropriate employer accommodations, and availability of language translation services in the context of non-English speaking (“non-ELS”) plan participants and beneficiaries).
Historical Governmental Actions
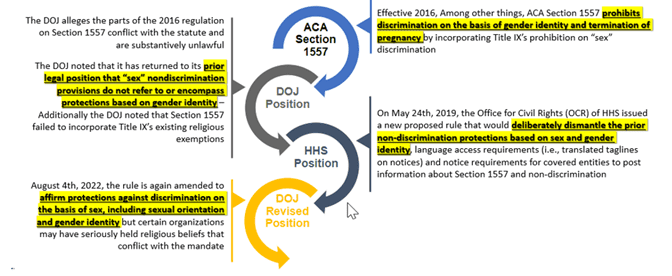
The Government modified its interpretation of Section 1557 interpretation on multiple instances. On April 5th, 2019, the Department of Justice (DOJ) filed with the Northern District of Texas their agreement with Franciscan Alliance v. Azar in which seven states and private plaintiffs alleged that part of the ACA Section 1557 rules were unlawful. Some states have imposed significant restrictions on treatments for gender dysphoria in minors, and not all courts agree whether Section 1557 extends to claims of gender identity related discrimination, which makes for a challenging compliance environment. The following graph illustrates a high-level path of Section 1557’s historical evolution and language changes over the last few years:
Key Provisions
The 2024 final rule expands the scope of prior 2020 regulations by providing that:
- Section 1557 applies to health insurance issuers, as well as all HHS-administered health programs and activities, which also touches health plan issuers via HHS-sponsored health programs, such as Medicare Part B, which is embedded in many healthcare initiatives and sponsored programs;
- Section 1557 provides protections against sex discrimination based on sexual orientation and gender identity, as well as sex stereotypes, sex characteristics, and pregnancy or related conditions; and,
- Nondiscrimination requirements apply to health programs and activities provided through telehealth services.
addition, entities covered by the final rule are required to:
- Notify individuals that language assistance services and auxiliary aids are available if needed;
- Take steps to identify and mitigate discrimination when they use patient care decision support tools; and
- Implement and train their staff on policies and procedures to ensure compliance with the final rule.
It is also important to point out that the final rule does not apply to employment practices, including the provision of employee health benefits.
Small Group Exemption
Section 1557 applies to groups with 15 or more employees, regardless of funding methodology or situs location. Section 1557 has been actionable law under the ACA since the ACA was established in 2010; consequently, if a plan has a total of 15 or more employees and is subject to the ACA, Section 1557 governs the health and welfare group programs sponsored by such employer.
Regulatory Notice Requirements
The final rule also requires covered employers to provide and post notice informing individuals of their civil rights under Section 1557. Further, Section 1557 requires that the covered health plan’s administrators have a civil rights grievance procedure, and they must identify (or designate) a named individual tasked with the coordination of compliance efforts for the plan, as well as for assuring remediation authority related to complaint proceedings.
Employers subject to the rule must also provide a notice informing individuals that free language assistance services and related auxiliary aids and services are available to protect individuals with limited English proficiency (“LEP”) and individuals with disabilities. The notice must be provided in the top 15 languages spoken by individuals with LEP in the relevant state or states where the entity operates. To minimize burden, OCR has prepared sample notices in English and 47 other languages that can be used if providers choose to do so. They are also free to create their own notices if they wish.
Additional Information & Related Resources
- Unpublished final rules from HHS:
- U.S. Department of Health and Human Services FAQs:
- Nondiscrimination in Health Programs and Activities under the ACA (1557) from Thomson Reuters:
- ACA Section 1557 Compliance for Health Coverage Toolkit from Thomson Reuters:
If you have comments, questions, or suggestions respecting the content of this ALERT or any other BRCC publication, please do not hesitate to reach out to the Baldwin Regulatory Compliance Collaborative at the following address:
[1] Note that the more narrowly interpreted 2020 final regulations failed to include rules related to discrimination as to gender identity and pregnancy termination, resulting in high profile politicization of the definition of sex and pregnancy termination. Further the 2020 rules did not include language for the health care coverage for gender identity.
For more information
We’re ready when you are. Get in touch and a friendly, knowledgeable Baldwin advisor is prepared to discuss your business or individual needs, ask a few questions to get the full picture, and make a plan to follow up.
This document is intended for general information purposes only and should not be construed as advice or opinions on any specific facts or circumstances. The content of this document is made available on an “as is” basis, without warranty of any kind. The Baldwin Insurance Group Holdings, LLC (“The Baldwin Group”), its affiliates, and subsidiaries do not guarantee that this information is, or can be relied on for, compliance with any law or regulation, assurance against preventable losses, or freedom from legal liability. This publication is not intended to be legal, underwriting, or any other type of professional advice. The Baldwin Group does not guarantee any particular outcome and makes no commitment to update any information herein or remove any items that are no longer accurate or complete. Furthermore, The Baldwin Group does not assume any liability to any person or organization for loss or damage caused by or resulting from any reliance placed on that content. Persons requiring advice should always consult an independent adviser.
The Baldwin Group offers insurance services through one or more of its insurance licensed entities. Each of the entities may be known by one or more of the logos displayed; all insurance commerce is only conducted through The Baldwin Group insurance licensed entities. This material is not an offer to sell insurance.






